If you are reading this blog post, chances are that you have been searching for answers regarding that frustrating pain you have been experiencing in the front of your hip.
While there are many things that may contribute to this type of hip pain, one of the most likely culprits is known as hip impingement, or femoroacetabular impingement (FAI).
It is often diagnosed in active people in their 20s, 30s, and 40s. Yet, it can occur in athletes and non-athletes alike. Hip impingement can limit performance, and sprint speed, and even make normal daily activities difficult to do. The symptoms of hip impingement can vary from person to person but tend to arise gradually, over days, weeks, and months.
Here are a few things you can look for:
- “Sharp” or a “pinching” pain in the hip crease or groin, and in some cases a stubborn “dull ache” in the back, bum, hip flexor, or thigh.
- Stiffness, weakness, and/or a decrease in the range of movement in the hip joint.
- Symptoms are felt most after sitting for long periods of time, during movements where your hip is near its end ranges such as during a deep squat, deadlift, going upstairs, or during sports that involve repetitive changes of direction and pivoting.
- Pain in the hip and groin can be intermittent and felt both during/after activity and/or at rest.
- In athletes, pain often affects performance and sprinting.
In some cases of hip impingement, hip pain and other symptoms may cause a person to walk with a limp. Some individuals may also experience a loss of balance, where balancing on the affected leg may be more difficult than balancing on the unaffected leg.
If this sounds familiar to you, you may be experiencing hip impingement or FAI. Rest assured that you are not alone. This is fixable!
FAI is a technical name that is used to describe naturally occurring differences, or changes, in the anatomy (or what we often call “morphology”) of the hip. These boney changes are normal yet can cause pain in some individuals. Not all individuals with these changes would experience symptoms or pain. In this blog post, we will help you understand how to manage symptomatic hip impingement with treatment and exercises!
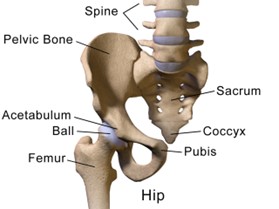
Hip impingement involves a change in the shape of the surface of the hip joint. Your hip joint is a ball-and-socket joint, where the “ball” (femoral head) is the rounded top of the femur. This is commonly known as the thighbone. The “socket” is called the acetabulum and is part of your pelvis.
There are 3 different types of bony changes to the hip joint that may describe your cranky hip. The first is known as Cam morphology. This happens when the femoral head (the “ball”) is shaped differently due to excessive bone growth. This part of your hip should be smooth and spherical; however, extra bone growth can form a bump on the “ball”, which can affect how the femoral head rotates (pointing the toes inward and outward) and moves in its socket. This type of hip impingement is more common in young men (Guyton, 2013).
The second type of hip impingement is called Pincer morphology. This occurs when excessive bone grows on the edge of the hip socket. This extra bone creates an overhang, making the socket deeper in certain places, which can prevent the femoral head from moving smoothly in its socket. If we were to think of your hip socket as a soup bowl, think that the bowl is deeper than desired.
The third type is called a Mixed morphology and is when there is a combination of the two. In this case, there could be extra bone growth both on the “ball” and around the “socket”. Learning these variances and the hip anatomy can help you to understand what may be going on inside your hip joint.

Now, if you have one of these variances, it does not mean that you need to panic or feel like you are guaranteed to experience pain. Morphology does not equal pathology. In other words, this means that even though your anatomy may be slightly different from what a textbook may consider “normal,” these changes are common and do not always cause pain or impingement symptoms. In fact, studies show 30% of individuals without pain or symptoms can also have these bony changes on imaging! It also means that corrective surgery is not necessary in most cases.
How is hip impingement diagnosed?
During the initial appointment of your injury, your therapist will ask questions to gain a better understanding of your symptoms and will then use tests and measures during their assessment. If you do not experience symptoms, it is unlikely that you do not have hip impingement. Additionally, your therapist will also assess your hip range of motion and compare this to your non-affected hip. An emphasis is placed on hip internal rotation (pointing toes inwards) and hip flexion (bending of your hip). Along with your symptoms and clinical findings, imaging is necessary to confirm a diagnosis FAI. X-rays and an MRI may be performed to identify changes in the shape of your hip bones. Symptoms AND clinical signs, in addition to imaging findings, are all required to make the diagnosis. Again, this is because it is common to have changes on imaging without any symptoms.
What is the treatment for hip impingement?
Physiotherapy is the primary course of action here, however not all physiotherapy is the same, it won’t get better with manual therapy and needles, it has to be an exercise-based approach, so you need a physiotherapist who uses strength and conditioning as their main focus. Surgery should be avoided wherever possible and used only as a last resort. Physiotherapy for hip impingement focuses primarily on exercise rehabilitation, activity modification, and some manual therapy. Rest and stretching are not enough to recover from this type of hip injury. There are several reasons why surgery is not recommended. The first is because outcomes tend to be similar at the 8-12 months mark in those who only used physiotherapy versus those who had surgery. After 2-years, there is no significant difference between those who had surgery and those who did not. The second reason is that surgery does not guarantee a return to normalcy or sport. According to a 2018 study that looked at individuals who opt for surgery when diagnosed with hip impingement, roughly 57% go back to playing their sport at their pre-injury level, and only 17% return to their prior level of performance. Like other medical procedures, there are also more associated risks when opting for surgery. These can include infection, nerve injury, fracture, dislocation, and death to name a few. Studies have even identified a significant increase in seven types of comorbidities like chronic pain and sleep disorders in individuals between the ages of 18-50 years within 2-years after hip arthroscopy surgery. Another factor to consider is the monetary cost. Surgery has a higher cost and is more expensive than choosing to do only physiotherapy. Lastly, it is important to note that three to six months of physiotherapy must be done after having the surgery. In other words, the surgical procedure for hip impingement is not a quick fix for getting out of pain.
Regardless if you take the surgical or non-surgical route, the two main aspects of treatment we focus on are load management and activity modifications. In the clinic, we determine your baseline level of tolerable activity and create a plan that gradually progresses you towards your goals. Tolerable activity essentially means the amount and type of physical activity that you can comfortably perform. For example, if you are an athlete who is unable to play your sport or run, we work to maintain your fitness through activities that are tolerable such as walking, cycling, strength training, and any other activity that keeps you moving without aggravating your hip pain. A large component in the treatment of hip impingement includes exercise rehabilitation with a heavy focus of improving the available range of motion in your hip joint and increasing the level of strength in the muscles that surround your hip. In fact, many patients who experience hip impingement symptoms tend to have reduced levels of hip muscle strength and balance. Improving the strength of these muscles not only helps to make them stronger but helps to decrease both stiffness and pain, as well as increase sports performance. Rehabilitation should emphasize hip muscle strengthening 2-3 days per week for at least 3-months. If you are an athlete or have a goal to return to a sport that requires running, jumping, sprinting, cutting, kicking, or pivoting, these activities along with plyometric and sport-specific exercises must be gradually incorporated into your training and rehabilitation program to ensure that you are prepared to return-to-play. The process needs to be progressive and individualized. This means the treatment plan continues to challenge you as your symptoms improve and is unique and specific to you.
In summary
Hip impingement (FAI) is a motion-related disorder of the hip with a triad of symptoms, clinical signs, and imaging findings. Hip impingement can be slow to be diagnosed. Symptoms can be frustrating and really affect your ability to do daily tasks and sports performance.
In most cases, exercise rehabilitation is the first-line recommendation of treatment for recovery from this injury. An emphasis on load management and activity modifications is essential. Hip strengthening exercises should be performed at least 2-3 days per week for a minimum of three to six months. It is important to understand that if you are an athlete or have a goal to return to a sport that requires running, jumping, sprinting, cutting, kicking, or pivoting, these activities along with plyometric and sport-specific exercises must be gradually incorporated into your training and rehabilitation program to ensure that you are prepared to return-to-play. Lastly, doing the right things is key. Stretching and resting are not enough. Surgery should be avoided wherever possible and used only as a last report. Your treatment plan should progressive and specific to you.
Check Out our Youtube Video where Kait explains more about Hip Impingement, watch it here
If you would like to find out more about your own hip pain, come see us in our Lucan Clinic, you can contact us here

